Definition and Causes of High Ankle Sprains

A high ankle sprain, also known as a syndesmotic sprain, occurs when the ligaments connecting the two lower leg bones, the tibia and fibula, are stretched or torn. Unlike traditional ankle sprains, which typically involve the ligaments on the outer side of the ankle, high ankle sprains affect the ligaments above the ankle joint, near the shin. These injuries often result from sudden twisting or rotational movements of the foot, such as those experienced during sports activities like football, basketball, or skiing. Additionally, direct blows to the lower leg or excessive force applied to the ankle can also cause high ankle sprains. Athletes and individuals with poor balance, weak ankle muscles, or previous ankle injuries are at higher risk of experiencing high ankle sprains. If you have sprained your ankle, it is suggested that you seek the advice of a podiatrist who can determine what type of sprain it is, and offer appropriate treatment solutions.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Peter Siroka, DPM from Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Common Classifications of Ankle Fractures

Ankle fractures often result from trauma or sudden twists during activities like sports or falls. These fractures are classified based on the location and severity of the break, aiding medical professionals in determining the most appropriate treatment. One common classification system divides ankle fractures into three main categories, which are lateral malleolus fractures, medial malleolus fractures, and posterior malleolus fractures. Lateral malleolus fractures involve the outer bone of the ankle, known as the fibula, and typically occur from rolling the ankle outward. Medial malleolus fractures affect the inner bone of the ankle, called the tibia, and result from inward rolling of the ankle. Posterior malleolus fractures involve the back of the tibia near the ankle joint and are often associated with high-energy injuries. If you have fractured your ankle, it is suggested that you confer with a podiatrist who can effectively diagnose and treat this condition.
Broken ankles need immediate treatment. If you are seeking treatment, contact Peter Siroka, DPM from Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
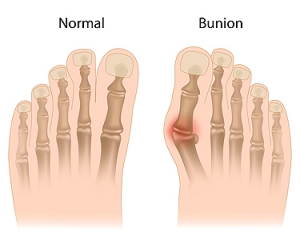
Key Facts About Bunions

Bunions, a prevalent foot deformity, are characterized by a bony bump that forms at the base of the big toe. Contrary to common belief, bunions are not merely a cosmetic issue but can cause discomfort and affect mobility. One essential fact about bunions is their tendency to develop gradually over time, often due to structural issues in the foot, such as flat feet or abnormal bone alignment. Additionally, wearing ill-fitting shoes, particularly those with narrow toe boxes, can exacerbate bunion development or worsen existing symptoms. Individuals with bunions may experience pain, swelling, redness, and restricted movement in the affected toe. Despite popular misconceptions, bunions cannot be permanently corrected through nonsurgical means. However, conservative measures such as wearing supportive footwear, and using orthotic inserts can help alleviate symptoms and slow the progression of the deformity. For severe cases causing significant pain or hindering daily activities, surgical intervention may be necessary to realign the affected joint and provide lasting relief from bunions. If you have a bunion, it is suggested that you are under the care of a podiatrist who can help you to manage this condition.
If you are suffering from bunions, contact Peter Siroka, DPM of Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
See Your Podiatrist Regularly If You Work On Your Feet
Understanding Corns and Their Causes

Corns, a common foot ailment, refer to thickened areas of skin that develop in response to pressure or friction. These small, round, or cone-shaped growths typically form on the toes or feet, causing discomfort and pain. The two primary types of corns are hard corns and soft corns. Hard corns, also known as heloma durum, form on dry, firm areas of skin, often on the tops or sides of toes. Soft corns, or heloma molle, develop between the toes where the skin is moist, appearing white and rubbery. Corns develop as a protective mechanism against repeated pressure or friction, commonly caused by wearing ill-fitting shoes, high heels, or excessive walking or running. Additionally, foot deformities like bunions or hammertoes can contribute to corn formation. Understanding the medical terminology associated with corns and their underlying causes is essential for effective treatment and prevention strategies. Corns on the feet can be painful. If you have developed this foot condition, it is suggested that you visit a podiatrist who can offer you effective relief techniques.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Peter Siroka, DPM of Connecticut. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
The Impact of Obesity on Adult Foot Structure

Obesity, a prevalent health concern worldwide, exerts a profound influence on foot structure and function in adults. The increased body weight places excessive pressure on the feet, altering their biomechanics and leading to various structural changes. One notable effect is the flattening of the arches, known as pes planus or flat feet, due to the increased load-bearing capacity required to support the body. This condition can contribute to foot pain, fatigue, and discomfort while walking or standing for prolonged periods. Additionally, obesity may worsen existing foot conditions such as bunions, hammertoes, and plantar fasciitis, further compromising foot health and mobility. Furthermore, the accumulation of fat tissue in the feet can result in swelling, inflammation, and decreased flexibility. Addressing obesity through lifestyle modifications, including diet, exercise, and weight management, is essential for mitigating these structural changes and alleviating associated foot problems. If you are experiencing any type of foot pain due to excess weight, it is suggested that you schedule an appointment with a podiatrist.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Peter Siroka, DPM from Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.